Despite systemic administered therapies, some patients with inflammatory arthritis continue to have chronic or recurrent joint inflammation in one or a few joints. Intraarticular glucocorticoids are often used with success in these patients; however, injections often have to be repeated periodically and there are concerns for the long-term consequences of injected glucocorticoids. Intraarticular injection of anti-TNF therapy is an attractive, but largely unstudied, option, as these agents have been shown to be very effective in reducing the disease activity of a number of chronic inflammatory conditions. In this proof-of-concept study, van der Bijl et al (Arthritis Care & Research 2009; 61(7): 974) explore the efficacy and safety of intraarticular infliximab compared to intraarticular methylprednisolone.
Methods
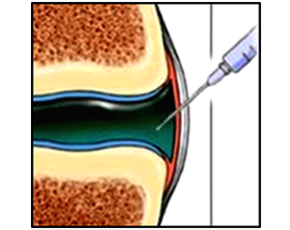
Adult patients without infection, gout, or osteoarthritis with a chronically inflamed knee despite one or more steroid injections within the past year were randomized to receive either an intraarticular injection of infliximab (100 mg) or methylprednisolone (80 mg). A second injection (randomly assigned) was given for recurrent symptoms within 3 months. Inefficacy was defined as the need for any retreatment (injection or surgical) at the 3 and 6 month follow-up visits. In all patients, aspiration was performed prior to injection by an investigator blinded to treatment allocation. The remaining investigators, study staff, and the patients were blinded to treatment allocation.
Results
A total of 23 patients were treated, with a total of 28 knees injected (15 knees were randomized to receive their first injection with infliximab and 13 with methyprednisolone). Inefficacy was noted in all 15 knees initially randomized to infliximab. Of these, 1 was reinjected with infliximab (not effective) and 8 were injected with methylprednisolone (1 of 8 effective). Of the 13 knees initially randomized to methylprednisolone, 7 were ineffective. Infliximab was injected into 4 of these, with none determined to be effective. In total, none of the 20 injections of infliximab were deemed effective, compared to 8 of the 21 injections of methylprednisolone (38%; p=0.004 compared to infliximab). Time to failure after injection was more rapid for the infliximab treated knees considering only the first injections and all injections. Clinical characteristics did not differ according to treatment allocation. There were no treatment related adverse events in either group.
Conclusions
For patients with chronic knee inflammation, intraarticular infliximab was not an effective at reducing signs or symptoms of inflammation, or delaying the need for additional treatments. Intraarticular methylprednisolone was effective in only a fraction of patients.
Editorial Comment
Using injected TNF inhibitors as adjunctive therapy for single difficult to treat joints is a compelling hypothesis; however, the findings from this investigation are quite suggestive of the futility of this strategy. The reasons for the lack of improvement are not clear. It is possible that infliximab injected into the synovial fluid is not absorbed into the deep synovium, where many of the processes driving synovitis are located. Another possibility could be that the properties of the infliximab antibody itself facilitates, rather than abrogates, inflammation within the joint (although it is not indicated that patients had worsening of their joint inflammation after injection). Regardless of mechanism, the lack of any improvement with intraarticular infliximab in this trial should discourage practitioners from using this off-label treatment. While also not effective in many of the patients, intraarticular glucocorticoids remain an inexpensive and generally safe option. However, this study demonstrates that other treatment options are needed for patients with difficult to treat “stubborn” joints with persistent inflammation.

