Acute Lyme disease diagnosis
Many cases of Lyme disease are initially misdiagnosed. Lyme disease can be difficult to diagnose because early symptoms of fever, severe fatigue, and achiness are also common in many other illnesses. In addition, diagnostic blood tests are not always dependable, particularly in early disease. However, the round expanding red lesion rash is a unique sign that is more specific for Lyme disease, and many times a diagnosis can be made based on the tell-tale erythema migrans rash itself. Yet, it is important to understand that the erythema migrans rash is not always present or recognizable, and symptoms can fluctuate.
Recognizing the Lyme disease erythema migrans rash can be crucial to early diagnosis and treatment.
Think the Lyme disease rash is always a bull’s-eye? Think again.
Think it’s a spider bite? Think again.
Please refer to our poster of varied rash manifestations as a helpful Lyme disease rash identification tool. Please also review the information below:
Despite common belief, the tell-tale ring within a ring bullseye rash is only present in a minority of Lyme disease patients. Instead, the majority of Lyme disease rashes are uniformly red or blue-red and do not have a central clearing or bullseye. Sometimes the site of the tick bite is clearly visible in the center of this lesion. The erythema migrans rash is almost always round or oval and expands over days to a diameter greater than 2”. The Lyme rash is often confused with a spider bite, despite spider bites not expanding in this way.
Though less common, blisters may appear in the center of a Lyme disease rash and can be mistaken for a spider bite or the rash of shingles.
It is important to note that not all infected tick bites successfully transmit Lyme disease. Tick bite reaction may occur due to skin reactions to substances from the tick bite and may be confused with the rash of Lyme disease. Tick bite reactions may last days to weeks, but unlike the Lyme disease rash, tick bite reactions remain small, do not enlarge, and are not associated with fever or other systemic symptoms.
A typical tick bite site reaction is dime-sized or smaller and does not enlarge each day like the erythema migrans rash of Lyme disease.
Bacteria from the Lyme disease rash can disseminate through the bloodstream and create new erythema migrans skin lesions at other sites distant from the initial bite.
How do you diagnose the later stages of Lyme Disease?
Disseminated Lyme disease, due to unsuccessful or delayed treatment, can become disabling. The bacteria can leave the skin where it was initially inoculated by the tick and travel through the bloodstream to numerous systems of the body, primarily joints, heart, brain, muscles and the nervous system.
Late disseminated Lyme disease has a wide range of presentations including extreme fatigue, neuromuscular pain, joint pain, Lyme arthritis, cardiac problems, meningitis, headaches, cognitive impairment, and other central nervous system dysfunction. There are some distinguishable signs of later stage Lyme disease including facial palsy in the second stage, and swollen knees in the third stage that are somewhat specific for Lyme disease, but not absolutely, because there are also other causes of Bell’s Palsy and swollen knees. Cardiac problems can include carditis, life-threatening inflammation of the heart.
Diagnosis can be confirmed by serology blood tests which measure the antibodies that are formed by the immune system in response to the Lyme disease bacterial infection. Collection of cerebrospinal fluid by lumbar puncture may be indicated in neurologic cases that may involve the central nervous system.
Can you use a serology test to diagnose the first stage of Lyme disease?
Serology antibody tests are generally more helpful for second and third stages of Lyme disease than first stage Lyme disease. Antibodies take weeks to develop, and if the initial presentation of Lyme disease is in the early stage those antibody tests may be falsely negative because the immune system has not yet had enough time to produce antibodies. If a physician is suspicious of Lyme disease but cannot make a diagnosis by the rash, then the antibody test in that first stage should be repeated 3 to 4 weeks later since a Lyme disease diagnosis can be missed with a false negative test in the first few weeks.
The Centers for Disease Control and Prevention (CDC) recommends using a two-step testing process. If an ELISA test is positive or equivocal, it is then followed by a Western immunoblot test. Note, this antibody-based testing system can produce some false positive results and also high numbers of false negative results, particularly in early infection.
On July 29, 2019, the FDA cleared several Lyme disease serologic assays for use based on a modified two-test methodology, allowing a sensitive enzyme immunoassay (EIA) or immunofluorescence assay first test to be followed by a second EIA in place of a western immunoblot assay.
Unfortunately, since the immune response to borrelia is heterogeneous, current antibody-based diagnostics do not capture all cases. For example, antibody testing can be a problem in patients with early disease who are treated with antibiotics. In these cases, a follow up antibody test done after treatment may be negative and never turn positive.
A negative antibody test does not necessarily rule out Lyme disease and should always be considered in the context of a full health history and clinical assessment.
Current problems with Lyme disease diagnosis & patient care
- Diagnostic tests cannot yet accurately identify the earliest stage of Lyme disease when making the diagnosis is crucial.
- The rash is not always present or easily recognized
- Misdiagnosis and delayed diagnosis can make Lyme disease more difficult to treat and lead to prolonged and debilitating illness
- Early symptoms can be mistaken for a summer flu
- Lyme disease can involve several parts of the body, including joints, connective tissue, heart, brain, and nerves, and produce different symptoms at different times.
- Antibody testing done after early treatment may be negative and never turn positive for some cases
- Borrelia burgdorferi can evade our protective immune system and trigger immune system dysfunction.
- No reliable blood test is presently available to measure treatment success, necessitating close clinical follow up and improved physician education.
- Presently there is no vaccine to prevent Lyme disease available to humans.
What is the difference between this “indirect” blood diagnostic test and a “direct” test?
Direct diagnostic tests measure the presence of the bacteria directly and are much more reliable than tests looking for indirect measurement of antibodies that measure a person’s immune response to an infection. Lyme disease diagnoses and disease management would benefit from validated diagnostic tests that directly measure the infection such as a culture, PCR test, or antigen detection tests. Direct tests are vital to the management of other infectious diseases such as HIV, hepatitis C, strep, and COVID-19, but have not yet become widely available for Lyme disease.
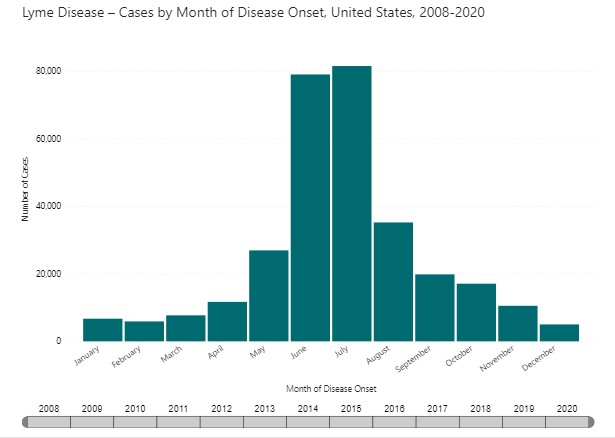
Does the time of year matter in the diagnosis of Lyme disease?
Since Lyme disease is a tick-borne infection, the seasonality of the disease is linked tightly to the life cycle and behavior of ticks. May, June, July, and early August are the biggest risk months for acquiring first stage Lyme disease in the US. This is the feeding time for nymph and adolescent ticks which are difficult to see. A viral-like illness in those early summer months might be Lyme disease. There is also some transmission of Lyme disease via adult ticks in the fall and winter and throughout the year anytime the temperature is above 40 degrees, but to a lesser degree.
The risk of acute Lyme disease is more of a year-round risk in more temperate regions such as northern California and the pacific northwest. Later stage Lyme disease, however, can manifest at any time.
Is Johns Hopkins trying to discover new ways to diagnose Lyme disease more directly?
Our Center is working on identifying biomarkers to improve diagnostics and to measure treatment success. Our research also supports the advancement of direct diagnostic tests to directly identify the Lyme disease bacteria.


